On September 28, 2023, one of the most prestigious journals of public economics, the Journal of Public Economics , published a research paper titled "The largest insurance program in history: Saving one million lives per year in China," by a research team from Massachusetts Institute of Technology (MIT), Xiamen University, and Peking University. The paper combines overall mortality rate data with individual survey data and examines the impact of China's New Cooperative Medical Scheme, considering its introduction and heterogeneity in rural areas.
1) Research Background
Healthcare expenditure risk currently stands as one of the major financial risks in developed countries worldwide. Virtually every developed nation has government or privately provided insurance plans that cover most of the population. Therefore, in 2018, across all OECD countries, the share of out-of-pocket healthcare expenditure was only 20.1% of total healthcare expenditure, accounting for 1.7% of income. In contrast, the coverage of health insurance among populations in developing countries is more fragmented. Traditionally, health insurance has not been a priority for development due to low healthcare quality and expenditure. For instance, in 2018, approximately 44.1% of healthcare expenditure in all low-income countries (LICs) was out-of-pocket, equivalent to 3.45% of income.
2) Research Motivation
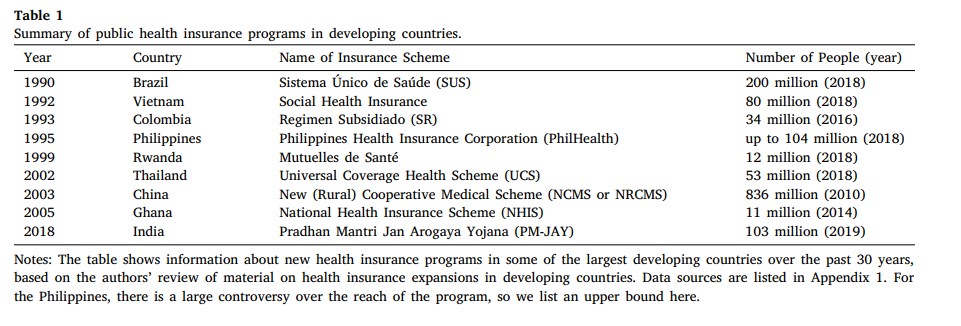
Public insurance programs in developing countries have expanded dramatically due to rising healthcare costs. Table 1 presents some of the largest new insurance schemes introduced in developing countries over the past 30 years, along with estimates of the number of people enrolled. The table shows that the largest expansion occurred with the introduction of the New Cooperative Medical Scheme (NCMS) in China in 2003. NCMS provided comprehensive coverage for inpatient expenses to rural households in China. Within its first eight years of implementation, it covered over 800 million people, making it the largest healthcare insurance program in modern world history. In 2015, NCMS expenditure accounted for 0.43% of GDP and 7.16% of healthcare expenditure. Despite being the largest insurance expansion in modern history, there has been little research assessing the impact of NCMS on health outcomes. Therefore, the authors conducted a comprehensive evaluation of the impact of NCMS on the health of rural residents in China. They combined data from various sources to analyze the effects of NCMS on mortality rates and other health outcomes, as well as its impact on healthcare utilization and expenditure.
3) Data and Methods
For baseline tests, the authors used data from the 2000 Chinese Population Census as the treatment variable and employed the China Death Surveillance Point (DSP) dataset to measure overall mortality rates. They collected data on the implementation dates of two rounds of the NCMS scheme. For the mechanism tests, the researchers utilized data on county-level healthcare supply (healthcare personnel and hospital beds) to examine potential mechanisms of supply response to NCMS, with control variables drawn from the 2005 to 2011 China Statistical Yearbook (county-level). For micro-level analysis, the researchers used data from the China Longitudinal Healthy Longevity Survey (CLHLS), which provided seven rounds of face-to-face interview data from 1998 to 2014 from 22 provinces in China, as well as data from the China Health and Nutrition Survey (CHNS) from 2000, 2004, 2006, 2009, and 2011.
In the process, the investigators found potential omitted variables closely correlated with the implementation timing of NCMS in the difference-in-differences (DD) estimation method, as well as the presence of non-parallel pretrends violating the identification assumptions of DD estimation. Therefore, they employed a richer empirical framework based on the classical overlapping DD model, allowing for the endogeneity of the timing of program adoption. The key innovation lies in recognizing an additional source of variation that previous analyses did not employ: the agricultural density of the county.
4) Results
The authors first used aggregated data on county-level mortality rates and life expectancy to obtain the intention-to-treat estimates of the health impact of NCMS. The study found that NCMS created significant health benefits for the rural population in China. By 2010, within eight years of NCMS implementation, 88% of the rural population in China and 62% of the total population nationwide were enrolled in the program. Since 2008, the authors estimated that NCMS has saved over 1 million lives annually, a number exceeding the population of seven U.S. states. The estimated cost per life saved is 66,000 RMB (approximately 98,000 USD), significantly lower than estimates of the statistical value of life in China and other measures such as compensation for accidental deaths.
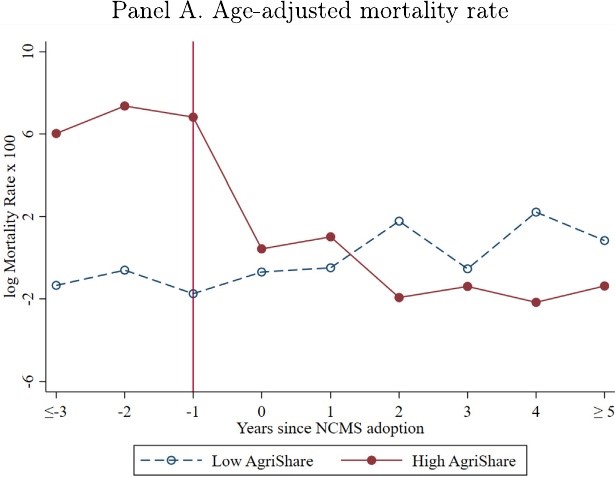
The figure above illustrates the mortality rates and life expectancy before and after the implementation of NCMS (subsampled by agricultural share), with both sets of counties exhibiting similar (relatively flat) trends before project implementation. The higher the level of urbanization in a county, the lower the mortality rate (by approximately 8%) and the longer the life expectancy (by approximately 1.5%).
Although in the year of NCMS implementation, mortality rates slightly increased and life expectancy slightly decreased in urban counties, mortality rates significantly decreased, and life expectancy substantially increased in rural countries. After reaching a new stable state in the following 2-3 years post-implementation, mortality rates decreased by approximately 4%, and life expectancy increased by approximately 0.7% in rural counties.
5) Micro-level Data and Mechanism Analysis
Micro-level data estimations suggest that the impact of NCMS on the mortality rate among the elderly is even greater than the value estimated in the total mortality rate data. The study also found that NCMS significantly increased healthcare utilization, with the probability of utilizing healthcare services increasing by 77%. Measurements of health status, such as limitations in daily activities, cognitive impairment, and self-/interviewer-assessed health status, also significantly improved. This confirms that the observed increase in life expectancy reflects broader health improvements and is consistent with the role of hospitals as a nexus of care in the modern Chinese healthcare system.
Next, the authors explored two mechanisms that led to these results. The first mechanism is related to out-of-pocket expenditures, with a significant decrease in very expensive out-of-pocket expenses. The reduction in out-of-pocket expenses resulting from NCMS enrollment may alleviate individuals' concerns about future health expenditure risks, potentially improving their mental health. Additionally, reducing out-of-pocket expenses can free up resources for other forms of consumption such as food, thereby contributing to improved health outcomes. The second mechanism is related to supply expansion, where the authors included supply controls in the outcome model, controlling for two supply indicators: the number of healthcare personnel and the number of hospital beds per 1000 people. The study suggests that an increase in supply does lead to a reduction in mortality rates and an extension of life expectancy. Furthermore, for every 10% increase in medical supply, mortality rates decrease by approximately 3%, and life expectancy increases by approximately 0.6%.
6) Conclusion
This article explains the significant impact of NCMS on health within the context of the healthcare system in China. Particularly, the inpatient coverage provided by NCMS plays a crucial role in general healthcare in China. Factors such as patients typically being referred from outpatient primary care clinics to hospitals, hospitals being widely used for the management of mild illnesses and chronic care, and the absence of charity care or uncompensated care in Chinese hospitals, also widen the potential for NCMS to have broad impacts on health.
7) Author Backgrounds

Yi Junjian is a distinguished professor at Peking University and a professor of economics at the National School of Development. He is also a dual-appointed professor at the Institute for Global Health and Development. He obtained his Ph.D. from the Chinese University of Hong Kong in 2011. From 2011 to 2014, he conducted postdoctoral research at the University of Chicago's Department of Economics under the supervision of James Heckman (Nobel Laureate in Economics, 2000) and Gary Becker (Nobel Laureate in Economics, 1992). From 2014 to 2020, he served as an assistant professor in the Department of Economics at the National University of Singapore. In 2021, he became an associate professor in the Department of Economics at the Chinese University of Hong Kong. Professor Yi is currently a distinguished professor at Peking University. His research interests focus on health and medical economics, big data analysis in healthcare and health, artificial intelligence economics, human capital theory, labor and population economics, development economics, econometrics, and behavioral economics. His research findings have been published in academic journals in the fields of economics, management, public health, and demography, including the Journal of Political Economy , Review of Economic Studies , Management Science , Demography , Lancet , and Proceedings of the National Academy of Sciences .

Jonathan Gruber is the Ford Professor of Economics at the Massachusetts Institute of Technology (MIT) and the director of the MIT Economics Department. Professor Gruber has been teaching at MIT since 1992 and has served as the head of the Health Care Project at the National Bureau of Economic Research and the president of the American Society of Health Economists. He is a member of the American Academy of Arts and Sciences, the National Academy of Medicine, the National Academy of Social Insurance, and the Econometric Society. He has published over 180 research articles, edited 6 research volumes, and authored books including the undergraduate textbook Public Finance and Public Policy , the graphic novel Health Care Reform , and Jump-Starting America: How Breakthrough Science Can Revive Economic Growth and the American Dream (co-authored with Simon Johnson).

Lin Mengyun is an assistant professor at the School of Economics at Xiamen University. She earned her Ph.D. from the National University of Singapore. She has published articles in journals such as the Journal of Public Economics , Education Economics , and China Economic Review .
(Interpreted by Waverly Shi)