ORCHA stands for the Organization for the Review of Care and Health Applications. The mission of ORCHA is not to review and improve digital health, but to deliver high quality digital health tools to people and patients. To achieve the mission, the first question is which digital health tools are of high quality. Therefore, I will introduce the work we have been leading on a global scale and share with some of the lessons.
Before I do that, I would like to start by setting the scene. You may be surprised to know that we currently have access to over 375,000 digital health apps. When I use the word app, I'm talking about apps that you can find in the app stores, but that also includes web-based solutions. Globally, 5 million people download one of these solutions every day. That has increased by 25% since COVID. Thus, what we have been seeing is that more people are really interested in how digital health can help their health or to help them with the health condition they may be living with.
It is also interesting to note the way in which our healthcare professional communities are also engaging with digital health. More than 80% of healthcare professionals are already using many medical apps on their smartphones and more than 40% believe that these tools could reduce the number of visits to the doctor's office. Surprisingly, over 90% of healthcare professionals believe these tools could improve the health outcomes of their patients. Currently, there are more smartphones on the planet than there are toilets and toothbrushes. The landscape reveals that many people are already using solutions that healthcare professionals believe could help their patients, and our organization have brought the infrastructure.
Then the question arises, why have we not yet regulated and embraced this opportunity? There are four major barriers to the adoption of digital health apps. The first major barrier is awareness, people, patients, and healthcare professionals are not aware of the opportunity that exists. At present, approximately 6,000 digital health apps are available to support people with dementia, and around 20,000 are available for mental health. However, awareness amongst the population and healthcare professionals remains low, and unfortunately, the current training of healthcare professionals does not include the world of digital health.
Once people have built up an awareness of digital health solutions, the next barrier is access. Where do people go to find these tools? Probably an app store. If the word dementia is typed in the Apple app store on the phone, only two or three results appear, and it is difficult to access more options.
The ultimate barrier is trust if the user does find the tool. How can people trust this tool? How will the app deal with the data collected? Is the data stored securely? Is it clinically assured and ethical? Will it meet the personal preference needs? Unfortunately, trust is not warranted. The research by ORCHA has found that only 20% of digital health tools meet the quality criteria that were expected before either wanting to use it or recommending it to patients.
The fourth major barrier is ongoing governance. Assuming a clinician deploys solutions for patients, what happens if the solutions change? What if solutions change in an unsafe way? Digital health is changing all the time, presenting benefits as well as risks. How can we ensure that future risks are managed and governed? Those are the four main barriers that have really prevented us from utilizing the opportunity of digital health on a global scale. Then, how does ORCHA overcome these barriers?
It all starts with trust. Trust is the biggest barrier to our adoption of digital health. How do we overcome this barrier and how do we build trust in a system? There are a lot of regulations and standards in the world of digital health, but the regulatory landscape regarding digital health is a real puzzle because not all the regulations and standards are relevant to all the four segments, including data privacy, security, clinical assurance, and user experience. Some of the regulations relate to data privacy, some to data security, some to clinical assurance, and some to user experience.

The next challenge of this regulation puzzle is that new regulations are emerging all the time in these different areas. Then, the third challenge is, as not all digital health tools are the same, which of these regulations should be applied to which tools? Some digital health tools are basic, but some are highly complex, built on clinical algorithms and interpreted in clinical systems. Therefore, it varies which regulations meet the needs of which products. This is a real challenge. Globally, digital health frameworks have been created mainly at national levels. The frameworks for digital health are trying to make sense of this regulatory puzzle and create assessment frameworks or questions to evaluate products and assure products of compliance with these standards and regulations.
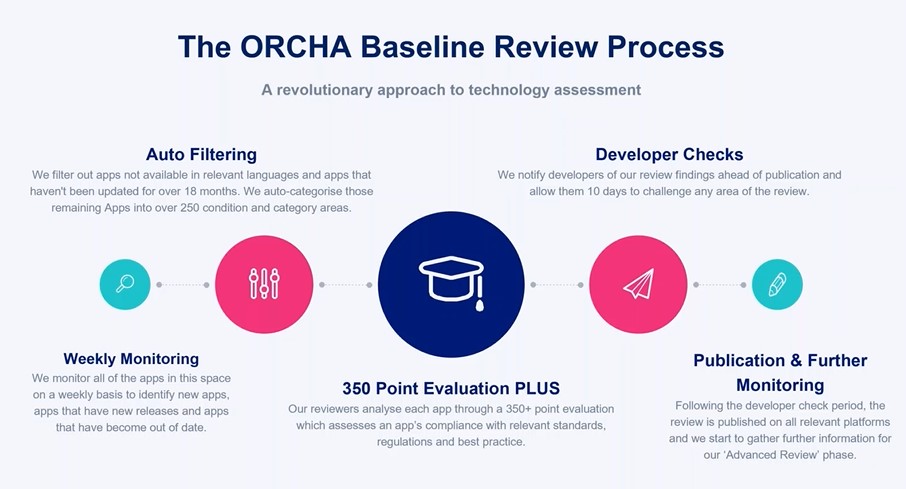
A lot of duplicated efforts may exist in these digital application assessment frameworks. ORCHA works globally to coordinate the baseline review assessment or the foundation review assessment. We have taken different duplicated standards and assessment questions on a global scale and pulled them into a foundational baseline review process. This is the ORCHA baseline review process, a robust process. It involves over 350 questions covering each of these four areas mentioned above. The beauty of it is that it is proportionate. We only ask relevant questions about the product that is being processed, and it is repeatable. This is important because the process is not just a snapshot of the view. This system is still a manual system, but it uses technology to support the process, and enables the review of every update and change of products. We also work with the developer to advise them on areas they may need to update and change to meet any regulatory requirements.
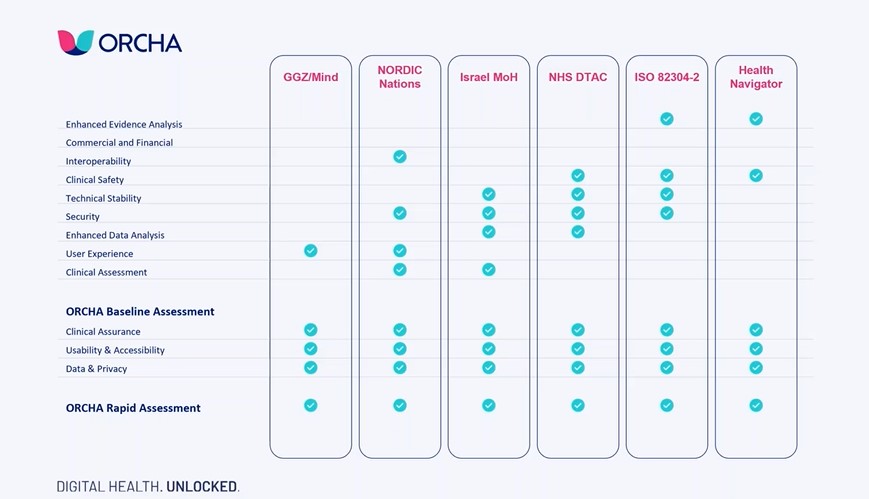
The work we are doing is based on the ORCHA baseline review. In the structure of the work, ORCHA's baseline assessment is at the bottom and the work carried out in different countries is at the vertical line.
The first one, we worked with GGZ/Mind (de Nederlandse ggz) on the project in the Netherlands and they were able to use all the work we have taken on the ORCHA baseline assessments. We, on their behalf, added additional questions and user experience to get approval in the Netherlands. In the five nations of the Nordic, they had different questions to ask in the review process, and we ran the answers through our system. We also had Israel, NHS (National Health Service) in the EU, ISO (International Organization for Standardization), Health Navigator in New Zealand. We also operate in other regions, such as Canada and America. This allows different regions to learn from each other in the process. We have processed 13000 digital health solutions through that ORCHA baseline assessment. We maintain a review of these products every time they are updated or changed, and then we need to add a few additional questions for specific jurisdictions. This means that the whole world can collectively learn from each other, and leverage the work that each other is doing.
Discerning good products is only the first step in truly helping patients become digitally able. Therefore, once we know which tools are safe and high quality that can be trusted, the next thing we need to do is simply tell people which ones are good. ORCHA has been working nationally, regionally, locally, or organizationally to create digital health app stores or digital health app libraries. These digital health libraries are promoted to specific communities of interest. Some of our libraries are focused on dementia, some others on adult mental health, and some others on long-term conditions. We work with these regions, nations, or organizations, to promote these libraries to people, so that people, communities, and patients know where to go to find a trusted solution. The libraries are equipped with highly configured and sophisticated search engines, which enable people not only to search for and find high-quality products, but also to filter them according to personal preferences and needs, for example, age, technological preferences, whether the individual has a hearing impairment or a visual impairment, what the individual wants from the project, etc.
In addition to these digital health libraries, we work with healthcare professionals who have touchpoints with the patients. The people who are interested in digital health are the truly activated communities. How do we activate those communities who are less activated to use digital health? The best way to activate people to use these tools and get the most benefit from these tools is to have trusted healthcare professionals recommend the tools to communities. We work with healthcare professionals, train them, and enable them to use these libraries as a formula. Doctors are very used to using formulas to prescribe medication. This is now becoming a digital health formulary approach where doctors, nurses, and therapists, can search for and find the right product for their patients and recommend it to them by a text message, directly to the patient’s phone.
Data suggests a conversion rate of around 71%. Approximately 71% of all people who receive the recommendation for a digital health tool via their healthcare professional will convert it and download it. This is not that dissimilar to the conversion rates of drug prescriptions. It means that people are able to access a high-quality digital health tool. It also means that because the back end is continuously re-reviewing and ensuring the quality of an ongoing basis, if we find a future fault with a product, we can do a recall, and that final barrier of governance and ongoing risk management are resolved.
It has been fascinating to look at the data behind the hundreds and hundreds of digital health libraries. We have been able to track what people have been searching for, for example, retrievals during the period of Coronavirus. This data is just a snapshot from March to December of 2020. In March, from the beginning of the pandemic, we saw a huge increase in the number of people and healthcare professionals searching for tools around respiratory conditions in COVID. That rapidly moved into a huge increase in mental health and then in the latter end of the year, towards diet and fitness.

It is fascinating just to observe the trends. I think what COVID has really given us is a real accelerator. As I have mentioned in the beginning, the number of people using digital health has increased by 25% to help themselves through the COVID crisis. Across the digital health libraries, we have seen a massive increase in people visiting and downloading tools. Referrals to patients by healthcare professionals have increased by 6500%. This means that our healthcare system is now much more ready to embrace the world of digital health and the opportunity of high-quality digital health.

Lastly, in order to really support the digital patients, we have to think about three key things. We must build trust in digital health, and that is why the review and robust review comes in. The second thing we must do is activate our populations and patients through our trusted partners, our healthcare professionals. We must enable strong governance and risk management, and use the data that comes out of digital health to feed the next steps.
[Liz Ashall-Payne, Co-founder and CEO, ORCHA]